The show today is a recording of an earlier conversation between Abby Burns and myself. This original conversation happened during the Raising the Value Bar Summit, which was a summit all about value and the what, why, and how of it all.
For a full transcript of this episode, click here.
If you enjoy this podcast, be sure to subscribe to the free weekly newsletter to be a member of the Relentless Tribe.
Abby asks me questions like why did I start the podcast, which fits the value theme because this show is entitled Relentless Health Value, after all.
I get asked how I define value. Fair question. Also, trick question, because value is in the eye of the beholder. All any of us ever have is a capability, a capacity.
The sorcery by which any given capability transmogrifies into value happens when somebody else’s problem or pain or need or want is solved for by said capability. Oh, you thought that was the tricky part? No, not in the healthcare industry. That’s probably the easy part, which is saying something, because product market fit is never easy.
The tricky part here is that in healthcare, as I’ve often said and heard, healthcare is an industry where one person eats the dinner, somebody else orders the dinner, and a third person pays for it. So, the patient may see immense value in whatever it is that somebody’s doing. But if the orderer and the payer don’t, well, the capacity is going to remain a caterpillar that never turns into a butterfly, most likely.
Said another way, the tricky part in healthcare is if you don’t create win-wins across a bunch of different boards, value won’t be realized for patients. And the problem with that is the number of zero-sum games we have afoot around here in the healthcare industry, which make this really difficult.
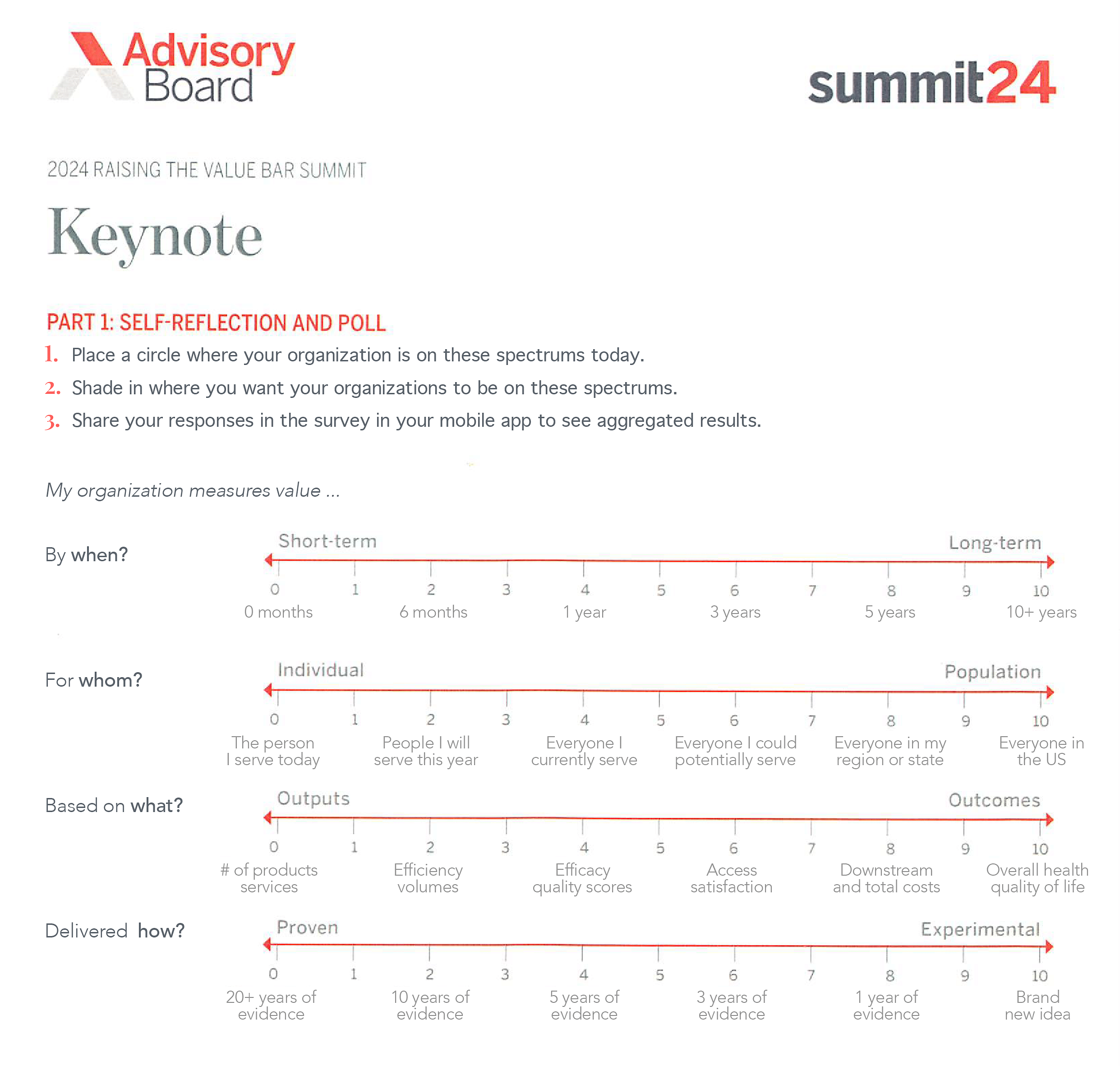
Before we kick into this show, I just want to mention, because it comes up several times in the conversation that follows, there was a talk by Daniel Kuzmanovich, who is managing director and expert partner over at Advisory Board. Daniel had given a talk earlier during that same value summit, and during this talk, he mentioned the idea that when measuring value in healthcare, there’s four tensions.
And if different stakeholders (or different people, actually, even within one stakeholder) have different perspectives on how value is created in light of these tensions, yeah, that’s where spheres collide and value drains away, never to be realized. So, the four tensions are:
Value Tension 1—When: By when must the value be realized? And some say that there is a tension between short-term value creation and long-term value creation. So that’s the first tension, this tension between somebody trying to get something done quick in the short term or only concerned about the short term and then what then happens in the long term.
Value Tension 2—Value for Whom: We could define this a bunch of different ways, but how Daniel defines it is the tension between individuals who are thinking one patient at a time and those who are thinking in terms of populations—could be populations of an organization; it also could be nationwide populations. Like, if I’m a doctor, do I worry about patients singularly or individually versus somebody thinking more top down from the population level down?
Value Tension 3—Value Based on What: And this tension could be, Are we thinking about value of the output, or are we thinking about the value of the outcome? Again, you’re gonna go about things kind of different ways if you’re thinking about output value versus if you’re thinking about outcome value. And, for sure, there could be tension if there’s not alignment there.
Value Tension 4—Proven or Experimental: People who only want to do things that are proven to drive value versus those who might be up for some experimental stuff. So, there’s this kind of tension between offering proven value and focusing on only things that are proven and evidence based versus those who are looking to incorporate experimental things into what they’re doing.
So, the tensions are when, short term, long term; for whom, patients or populations; based on what; and then lastly, is it proven or experimental?
Before we roll tape, I just want to thank Abby Burns, who is my interviewer today and a great one at that. She even managed to keep the likes of me mostly on track and on topic, which is no small feat. Thank you so much, Abby.
Abby Burns is an expert partner over at Advisory Board. She’s also a frequent host on the Radio Advisory podcast and a strategy lead.
Also mentioned in this episode are Abby Burns; Daniel Kuzmanovich; Scott Conard, MD; John Lee, MD; Mike Tuggy, MD; and Michael Leavitt.
For more information, go to Radio Advisory or Aventria Health Group.
Abby Burns is a researcher and facilitator with Advisory Board and serves as co-host of the Radio Advisory podcast. Through leading research and connecting with healthcare leaders both live and via Radio Advisory, Abby aims to provide meaningful thought partnership to help stakeholders across the industry to improve healthcare within and across their own domains. A self-avowed “healthcare generalist,” Abby’s research has a home base in health system strategy. She has previously led research on behavioral health, rural health, population health management (including primary care strategy and social determinants of health [SDOH]), and more.
Abby previously volunteered as an EMT in Prince George’s County, Maryland, where she regularly witnessed many of the challenges Advisory Board research aims to help members address. She earned her BA in public health from the University of Richmond.
Stacey Richter uses her voice and thought leadership to provide insights for healthcare industry decision makers trying to do the right thing each week on Relentless Health Value. Each show features expert guests who break down the twists and tricks in the medical field to help improve outcomes and lower costs across the care continuum. Relentless Health Value is a top 100 podcast on iTunes in the medicine category and reaches tens of thousands of engaged listeners across the healthcare industry.
In addition to hosting Relentless Health Value, Stacey is co-president of QC-Health, a benefit corporation finding cost-effective ways to improve the health of Americans. She is also co-president of Aventria Health Group, a consultancy working with clients who endeavor to form collaborations with payers, providers, Pharma, employer organizations, or patient advocacy groups.
03:33 Stacey’s journey and mission.
04:16 The story of Scott Conard, MD (EP391).
09:28 Why it’s important not just to drive change but to sustain it.
12:23 Heart Failure: A Case Study in Value.
14:13 EP438 with John Lee, MD.
15:07 Why patient positive value often fails instead of succeeds.
18:07 How financial toxicity has become clinical toxicity in healthcare.
19:44 How cultural norms have evolved into healthcare challenges.
23:38 The story of Mike Tuggy, MD, in Washington.
25:13 Looking at the four tensions in measuring value as continuums.
25:37 Why timeline is important in creative value in healthcare.
27:52 Finding Allies by Michael Leavitt.
28:34 What are the four ways to measure value in healthcare?
29:27 How do payers and providers collaborate to align on value metrics?
31:26 Why will proven versus experimental treatments become more important in the next few years?
34:54 Stacey’s manifesto (EP400) and values for personal integrity in healthcare.
38:55 Stacey’s parting advice.
Recent past interviews:
Click a guest’s name for their latest RHV episode!
David Muhlestein, Luke Slindee, Dr John Lee, Brian Klepper, Elizabeth Mitchell, David Scheinker (Encore! EP363), Dan Mendelson, Dr Benjamin Schwartz, Justin Leader, Dr Scott Conard (Encore! EP391)