David Contorno the other day posted the life expectancy chart comparing the US to comparable countries. Spoiler alert: It’s horrifying.
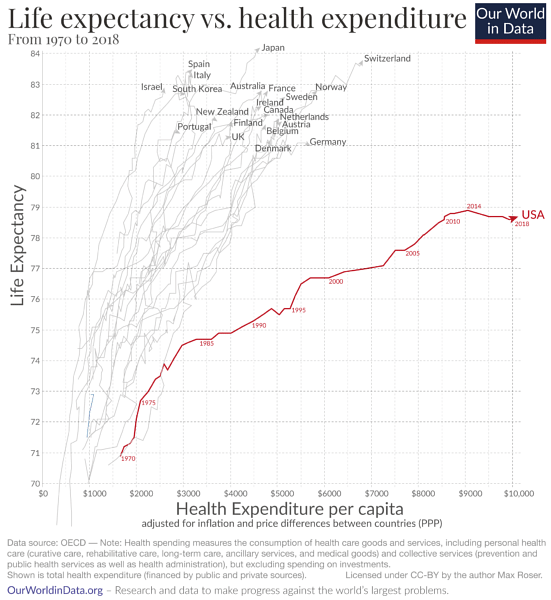
You see Japan; you see Switzerland, Israel, Spain, Italy … basically everybody else in a cluster of pretty darn vertical lines: increasing life expectancies year over year without much cost increase at all. And then—wow!—off to the right, all by itself, you see the USA, costing nearly double the worst of the other countries with a life expectancy that is years lower. We pay a whole lot, and despite all of the advances in medicine and how much we pay, we don’t seem to be getting the value for our dollar.
We could dig into those poor outcomes that we pay for. If we were going to, I might mention our truly beyond-upsetting maternal mortality rates and also infant mortality rates, which are way above other comparable countries. We could talk about all of our issues with diabetes and obesity. But let’s save all that for another day and just take one example that is really the quintessential example of what’s going on. Let’s chat about heart failure for just a sec. Here’s some stats for you. They come from Dr. William Bestermann’s Substack newsletter, and if you don’t subscribe to it, you might want to. It’s free.
Dr. Bestermann wrote: “Twenty-two percent of heart failure patients who are admitted to the hospital are dead within a year. Patients with [heart failure] generate a third of Medicare spending and 40% of Medicare fee-for-service deaths. Overall, heart failure patients have a mortality of 22%, compared [to] 4% for Medicare patients without heart failure. They are responsible for 55% of Medicare readmissions.”
But here’s some good news: In Denmark, investigators proved that using optimal medical therapy reduced heart failure admissions by 70% compared with usual care.
Here’s some more good news: There was a small, impoverished town near the coast of the Carolinas that had very few heart failure admissions. How did they accomplish that, you might wonder? Well, there was a nurse—one nurse—who was working under a grant. She was very dedicated. She had a list of all the heart failure patients in the area, and this was her job: making certain that every patient was on the best treatment for heart failure. She called the patients. She spent time with them. She had a trusting, caring, long-term relationship with them. That’s it! That was the secret sauce.
As Dr. Bestermann says, “Every poor community in our country could do that, but they don’t.”
So, this leads us to care gaps—dare I say, this country’s seeming care gap fetish dealing with care gaps retroactively.
In this healthcare podcast, I’m speaking with Carly Eckert, MD. It’s kinda funny, actually. I originally wanted to get Dr. Eckert on the show to talk about care gaps and how to close them, but this show did not wind up going how I thought it was going to go because Carly Eckert is a physician by training who got really interested in the upstream causes of what she was seeing in clinical practice. Despite my best efforts, she refused to be lured into my closing care gaps conversation. So, instead, this conversation is about the construct of care gaps and thinking about them in context. Closing care gaps is a model of care and maybe not a particularly great one, relatively speaking. In fact, here’s another name for the model of care called closing care gaps: care gap whack-a-mole. Care gap pops up … we whack it. Care gap pops up … we try to close it. Another care gap pops up … we try to close it. Another care gap … you get the idea.
Carly Eckert has worked in epidemiology and public health and also clinical informatics for health systems and payers. She is currently leading a team at Olive AI working on network data analytics and machine learning algorithms.
I recorded this show with Dr. Eckert prior to EP359 with Dan O’Neill. In that interview, which you should go back and listen to when you have a sec, Dan O’Neill cleared up a couple of things that I struggled with during this interview.
Here’s the big one that I could not figure out: Why with the whack-a-mole? Why do we still insist as a nation on waiting for someone to show up in clinic to retroactively and reactively address a missed preventative care opportunity?
Why don’t so many more provider organizations create pop health programs that consider the whole person proactively? Why don’t they take the time to operationalize whole-person care in a meaningful way? Why don’t they do what that nurse was doing in the Carolinas?
Ah, yes … to the surprise of exactly no one, it’s all about the Benjamins.
As Dan O’Neill put it, if all a provider organization is doing is slapping a sheet on a doc’s desk every morning with a list of care gaps for all the patients that he/she will see that day, it’s highly likely that incentives, or penalties to do anything else, are very weak. It’s a sign that, from a paying for value perspective, we’re not paying enough for value that it’s worth it or maybe even feasible for any provider organization to take the time and capital expense to switch up their business model in any meaningful way. So, the provider gets a little bump or a little knock if they don’t meet some quality standard. OK, great … so then they’ll minimally tweak their workflow and have doctors within their 7- to 15-minute visit suss out and try to close care gaps.
I don’t want to say this is entirely negative. It’s known that when provider organizations do close care gaps, patient outcomes do tend to get better—so, not arguing that. But there’s opportunities that get left on the table with all this reactiveness. Bottom line: You insurers, you purchasers of healthcare, get to it. Pay for value, for real. If you’re still just kinda paying mostly FFS with an icing of quality measures, maybe think a little bit harder about what’s next that’s really gonna end the whack-a-mole and bring about a more proactive and in-context mindset.
But you provider organizations, if you don’t fix this stuff yourself, you’re gonna get doctors and other clinicians (as we’re seeing) burning out and quitting because there’s only so much you can jam into a 7- or 15-minute visit, number one. But number two, doing population health reactively like this is suboptimal—and everybody knows it. So, what winds up happening is dedicated doctors and nurses desperately want to do the right thing but simply do not have the time. And they watch patient after patient suffer for it. That sucks. So, fix it. Maybe find a nurse like they did in North Carolina. At the end of the day, it’s probably cheaper to stand up a program like that than having to recruit all new doctors and hire traveling nurses when all of the current staff quits due to burnout and/or moral injury.
You can learn more at oliveai.com.
You can also connect with Dr. Eckert on LinkedIn and follow her on Twitter.
 Carly Eckert, MD, MPH, is a product leader at Olive AI, the automation company creating the internet of healthcare. As a trained physician, epidemiologist, and informatician, Dr. Eckert brings a tremendous amount of clinical experience and relevant healthcare industry knowledge to her work. In her role, Dr. Eckert combines her expertise, data understanding, and deep passion to impact healthcare for all patients. Prior to her role at Olive, Dr. Eckert led product for multiple AI start-ups with a particular interest in socially responsible technology and community impact.
Carly Eckert, MD, MPH, is a product leader at Olive AI, the automation company creating the internet of healthcare. As a trained physician, epidemiologist, and informatician, Dr. Eckert brings a tremendous amount of clinical experience and relevant healthcare industry knowledge to her work. In her role, Dr. Eckert combines her expertise, data understanding, and deep passion to impact healthcare for all patients. Prior to her role at Olive, Dr. Eckert led product for multiple AI start-ups with a particular interest in socially responsible technology and community impact.
06:59 What is the true goal in making population health successful?
07:26 How does the clinical pathway need to manifest in population health?
08:00 How do we get a nonfragmented state of care?
08:25 What is the best model of care?
10:08 “Identifying and addressing care gaps is an important element of population health.”
13:01 Closing care gaps vs creating a nonfragmented system of care.
17:11 “I think you have to take small steps with people.”
18:18 “There’s a lot of power in peer support.”
18:52 Why should provider organizations connect with peer groups?
20:39 “The key is that it’s not going to be the same for everybody.”
24:43 Why is diversity of the workforce key to closing care gaps?
25:07 EP322 with Monica Lypson, MD, MHPE.
25:11 EP347 with Ian Tong, MD.
30:09 Where can providers improve transparency to help close care gaps?




